This Mental Health Awareness Month, we’re raising awareness around engagement strategies and solutions that healthcare providers and payors can use to help patients and members living with mental or behavioral health conditions.
The impact on behavioral health in the U.S. has been exacerbated by the pandemic, economic anxiety related to inflation, rising consumer costs, and job insecurity. According to a 2022 CNN poll, 90% of respondents believe that America is experiencing a mental health crisis, with half of those surveyed saying that someone in their family has recently experienced a severe mental health episode. Additionally, 20% of respondents rated their own mental health as either “fair” or “poor.”
While demand for mental health services is growing, access to professional help is limited. The National Council for Economic Well-Being cites lack of access to care as a significant cause for the crisis, as more than 40% of Americans who reported seeking mental health care couldn’t get it. Compounding the issue is the correlation between poor mental health and poor physical health, as depression has been linked to a number of chronic illnesses, including diabetes and heart disease.
Healthcare providers and health plans have an opportunity to improve access to mental health services by implementing reactive and proactive patient and member engagement strategies for mental health.
Patient and Member Engagement Strategies for Behavioral and Mental Health
Here are three behavioral health strategies that Carenet can help your organization implement to help the mental wellbeing of your patients.
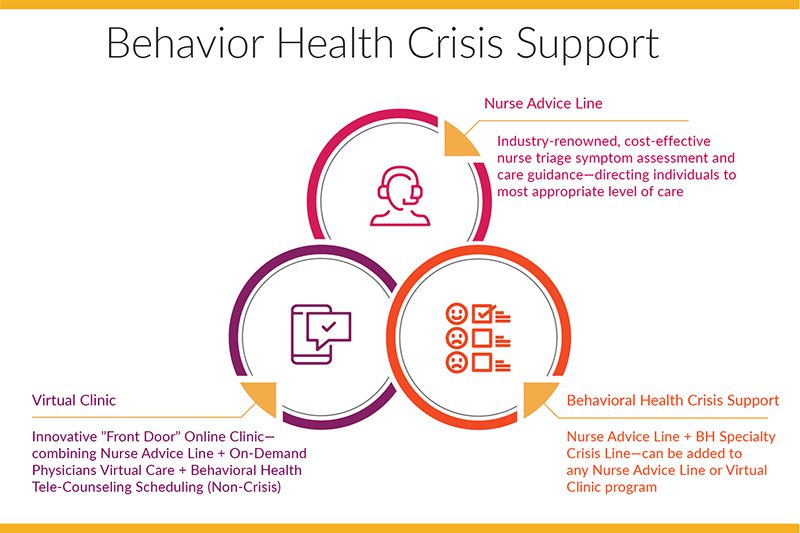
Behavioral Health Crisis Program
Behavioral health crisis support, in tandem with Nurse Triage and Advice Line, gives patients and members access to licensed behavioral health clinicians for immediate de-escalation and coordination of resources for longer-term solutions.
By including behavioral health crisis support in virtual clinics and nurse advice lines providers and health plans:
- Assess patient’s immediate need for support
- Guide patient to necessary support, resources and tools after assessment (including network providers, facilities and community resources)
- Promote use of available health and wellness services
- Evaluate patients for the presence of depression, anxiety, substance use concerns, interpersonal stress, and compliance with prescribed medications.
- Coordinate care for emergent and urgent situations
Support Patients at Home
Visiting the doctor can be overwhelming, especially when discussing behavioral or emotional health. For patients to feel comfortable opening up, building trust through communication is key. Providing behavioral and mental health care via telehealth services, and 24/7 advice lines is a great way to improve access and overcome stigmas and fear around in-person care.
Proactive Patient Outreach
Often, concern about a mental health diagnosis, as well as the associated assumed stigma, prevents people from seeking the emotional support services they need on their own. During Mental Health Awareness Month and beyond, providers and health plans can run outreach programs through social media, media, mail, phone, text and email to engage individuals in their mental health journeys. They can share important resources – like this article from the National Institute of Mental Health, which provide tips for talking with your healthcare provider about mental health. They can also invite individuals to schedule appointments, and to learn more about the resources available to them for behavioral and mental health. By communicating with patients where they’re most comfortable, and by opening the conversation, health organizations can help patients receive the services and support they need.
The Importance of Patient and Member Engagement Strategies for Behavioral and Mental Health
Data from the American Psychological Association shows Americans are becoming more open about mental health. What’s more, the majority of adults harbor positive associations with mental health treatment: 87% believe mental illness is nothing to be ashamed of and 86% believe people struggling with mental health disorders can get better.
While Americans are growing more comfortable talking about mental health, it’s still a pervasive issue. Tens of millions suffer from mental illnesses every year — an estimated 26% of adults over the age of 18 have a diagnosable condition. Throughout the pandemic, this number soared, with more people seeking treatment than ever before. However, estimates suggest only half of people with mental disorders receive treatment.
It’s more important than ever that providers and health plans are available for and engage with their patients and members to ensure they have access to the behavioral and mental health care they need.